How to Optimize Treatment with Insurance-Preferred Drug Replacements?
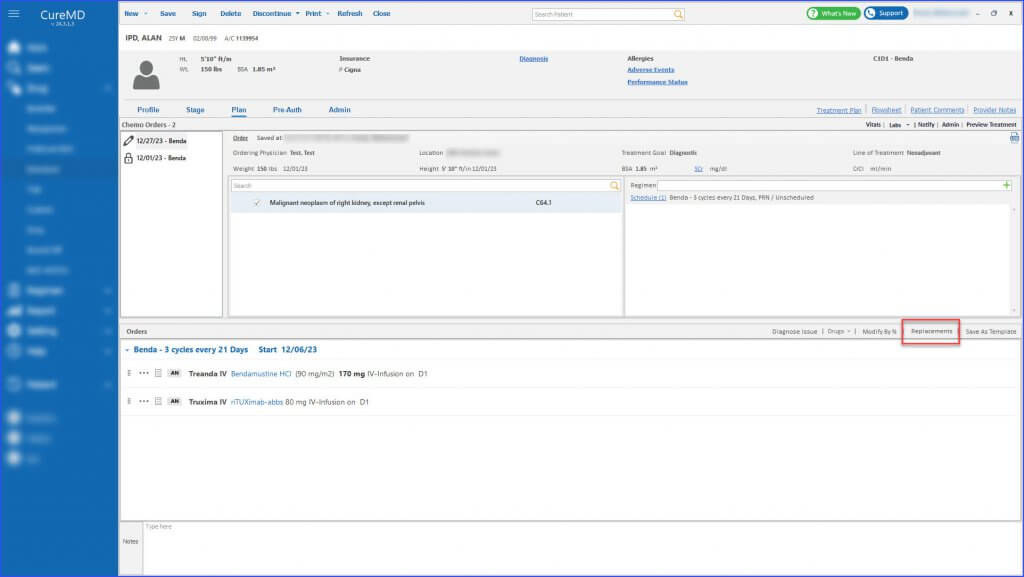
Users can manage and adjust chemotherapy treatment plans for their patients based on the changing preferences of insurance companies regarding medication. This enables the healthcare providers to easily update chemotherapy treatment plans with insurance-preferred drugs when insurance companies change their preferred drug lists.
Key Considerations:
- Scope: The feature scans for and suggests replacements for all drugs in the treatment plan, including those already administered (consumed) and those yet to be administered (unconsumed), taking into account various factors like biosimilars, brand vs. generic distinctions, and changes in administration routes.
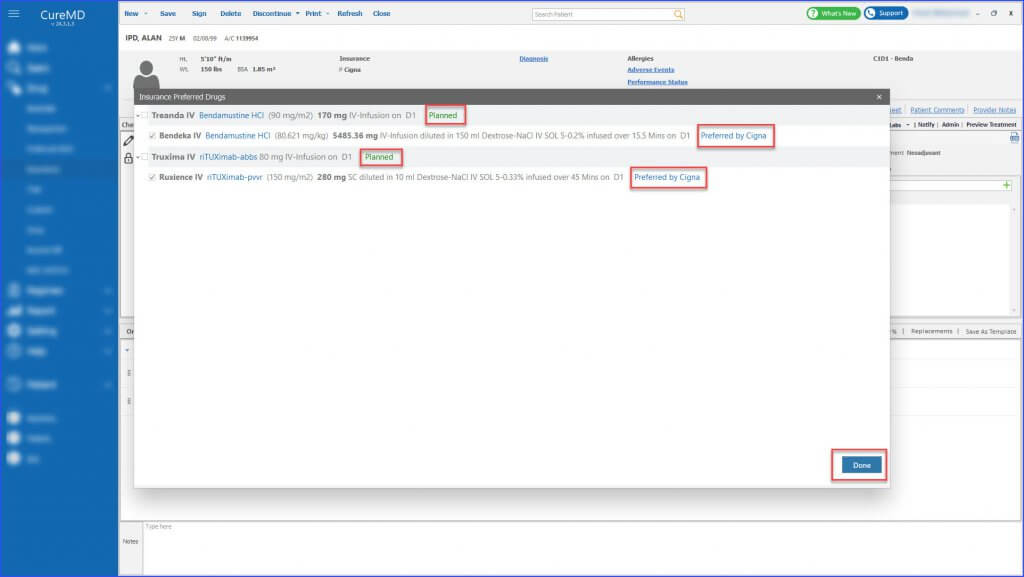
- Insurance Preferences: Only drugs that have insurance-preferred alternatives are flagged and offered for replacement. This ensures that changes are relevant and in full compliance with insurance policies.
- Flexibility: Users have the flexibility to choose from multiple insurance-preferred alternatives, allowing for personalized patient care that aligns with medical needs and insurance coverage.
Users can replace the current medications in a patient’s treatment plan with those preferred by their insurance, focusing on the transition from one brand to another, brand to generic drugs, or vice versa. This system ensures that when a drug is replaced due to insurance preferences, the historical data of drug consumption is preserved, reflecting the old medication on past treatment days and the new, replaced medication on future treatment days. Additionally, it incorporates a functionality to notify users when no insurance-preferred replacements are available in both brand vs generic cases.
Moreover, users can also replace current medications in a patient’s treatment plan with biosimilars preferred by their insurance.
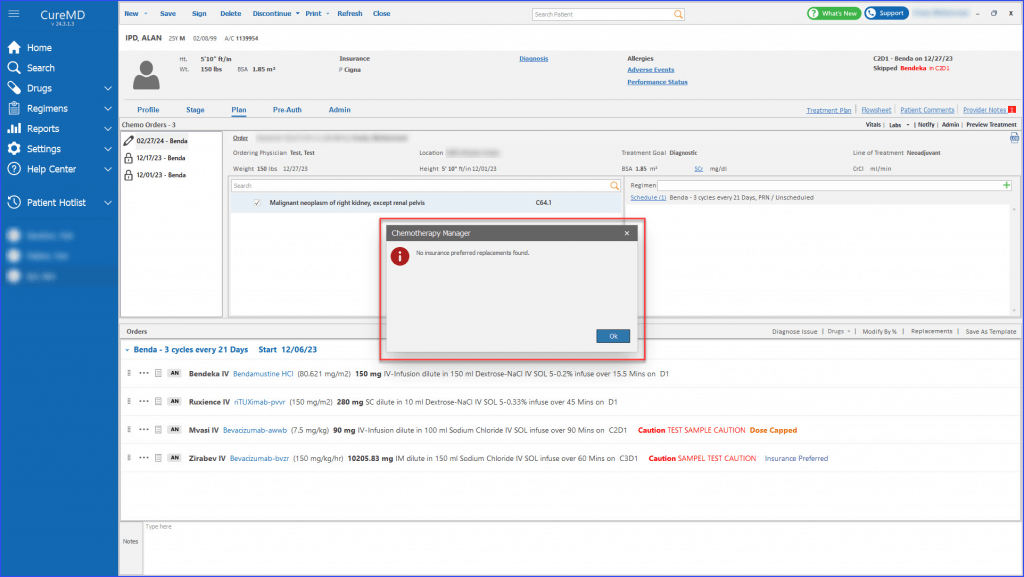
It ensures the continuity of the treatment by preserving the schedule of the previously consumed drug for the newly replaced biosimilar, while historical treatment data is updated to reflect the change. Critical to this process is the requirement that old pre-authorizations won’t apply to the new drug, and replacements can’t proceed for medications with outstanding, unconsumed treatment days, necessitating specific actions from the user. Additionally, it incorporates a functionality to notify users when no insurance-preferred replacements are available in biosimilar cases.
