What is Pre-Authorization?
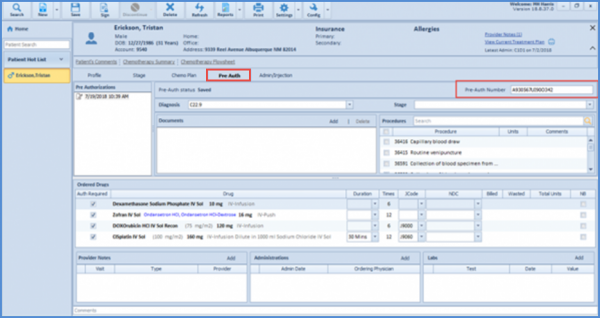
Pre-authorization is the medication pre-approval process used by practices. The information in the pre-authorization section is needed to send a complete request to the patient’s insurance company for prior authorization for a treatment or drug to be claimed later on.
It is an agreement by the insurance company to pay the claim for that approved medication when eventually received. After reviewing the pre-auth request, the insurance company can either accept or reject it. If approved, the insurance company provides a PAN – Prior Authorization Number that is recorded on the chart.