How to Select Eligibility Service Type at Plan Level?
User has the option to choose preferred service type at plan level.
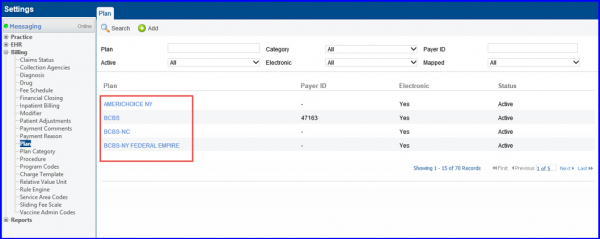
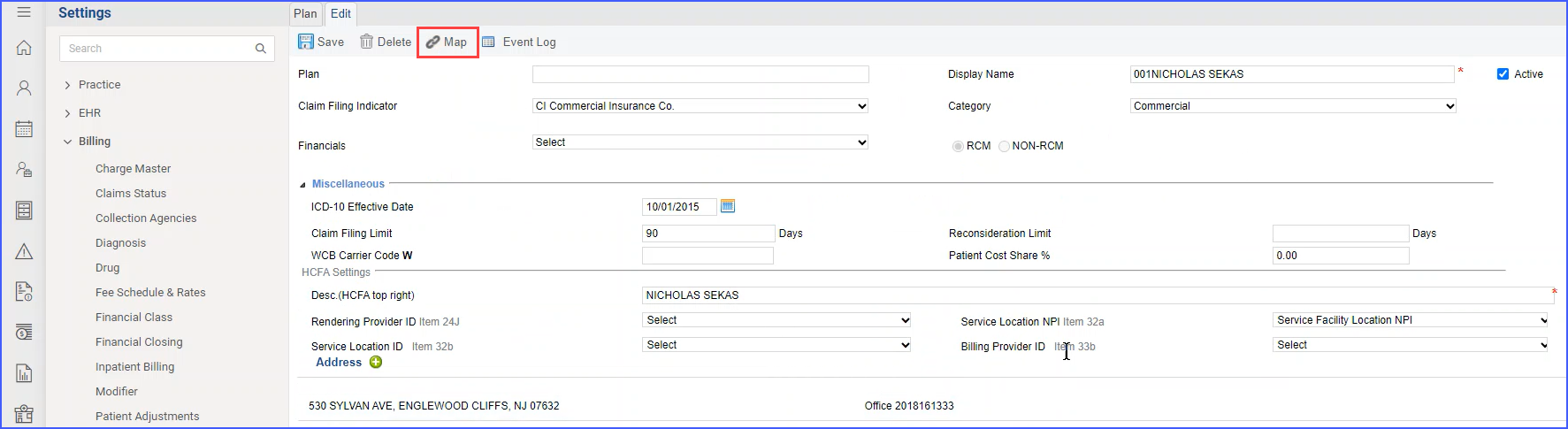
To do this, follow the above mentioned workflow and land on “Plan” page.
Once on “Plan” page, select a plan to edit it.
Editing a plan takes the user to “Edit” page. Here, expand ‘Miscellaneous’ and select multiple service type options from ‘Eligibility Service Type’ drop-down.
‘Eligibility Service Type’ drop-down is only visible for mapped plans.
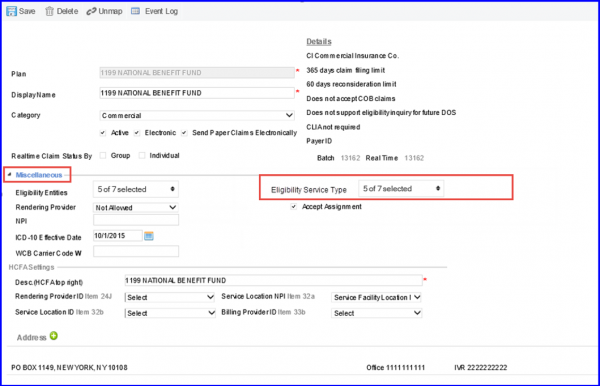
Service types selected here are visible on the patient insurance. To learn more about it, click here.
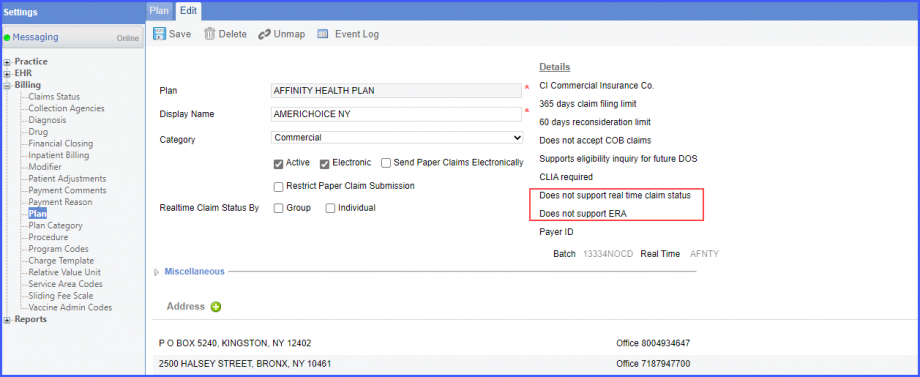
If an insurance plan does not support ERA and real-time claim status, then this information is mentioned in its details.
This helps billers in effectively managing the claims.
Select an insurance plan which does not support ERA and real-time claim status. Under the ‘Details’ heading, the system displays ‘Does not support real time claim status’ and ‘Does not support ERA’.
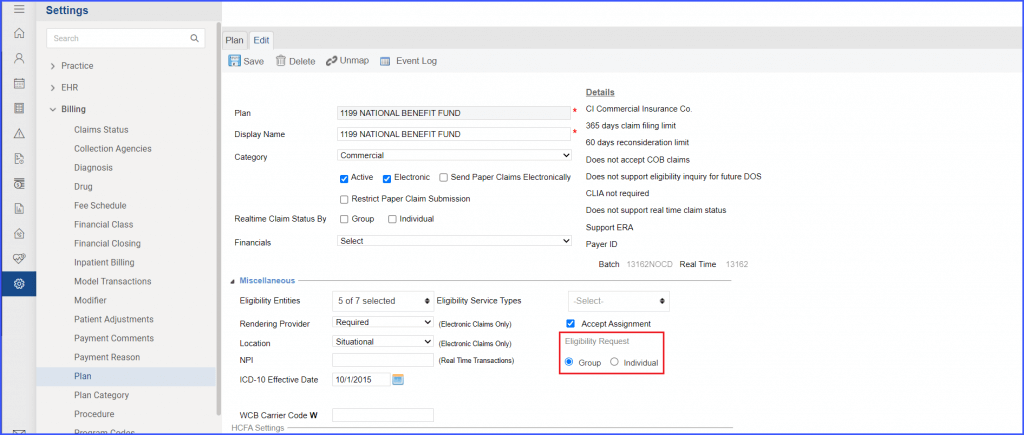
‘Eligibility request’ section has been added under the ‘Miscellaneous’ section with two radio buttons named ‘Group’ and ‘Individual’.
The ‘Group’ radio button is marked check by default.
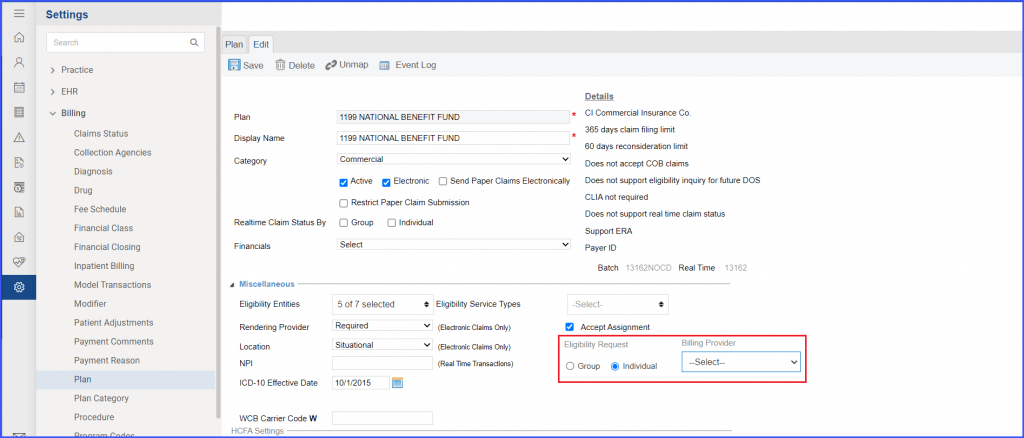
Meanwhile, if the user selects the “Individual” radio button, the ‘Billing Provider’ dropdown field appears on the right side. The “Select” option appears as the default choice and the user is required to select one billing provider from the list. If they proceed to click ‘Save’ without selecting a provider, the system displays an error message prompting the user to select an individual provider.
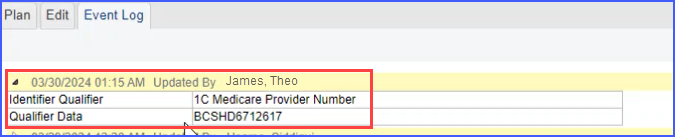
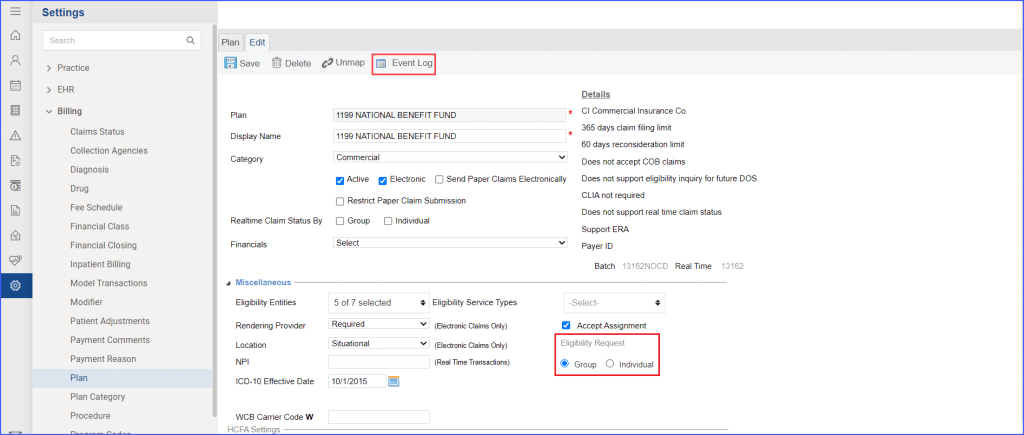
Adjustments made to the eligibility request settings are recorded in the ‘Event Log’ sub-tab on the ‘Edit’ page.
Once the user clicks the ‘Save’ button after making changes to the Eligibility Request settings, they can view the logs of the changes by navigating to the event log sub-tab at the top of the page.
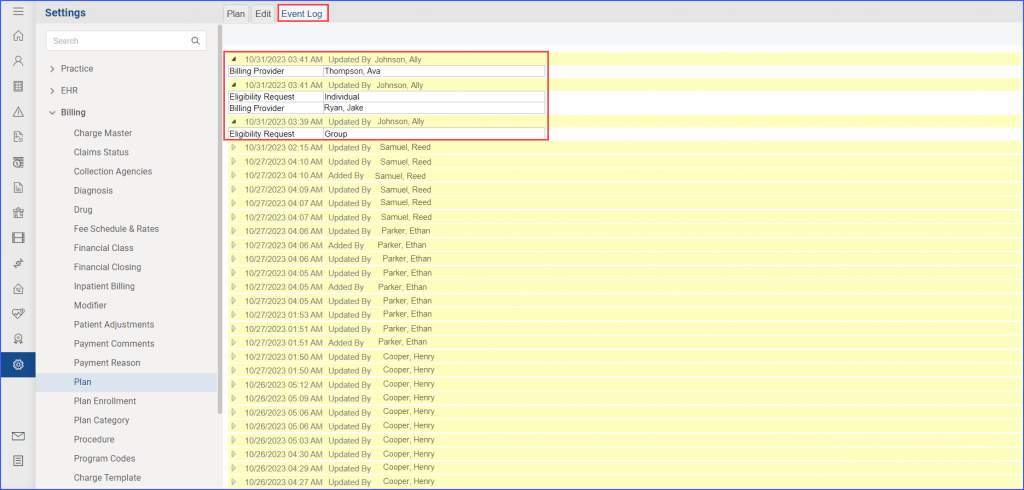
Here, a detailed record is maintained of any changes made to the eligibility request settings. The information displayed for these logs includes:
- Name of user who made the change
- Date and Time of change
- Specifics of the change made (individual or group)
- In case the ‘individual’ radio button is selected, the chosen billing provider is also shown.
Under the Miscellaneous section for Eligibility, the Information Receiver Additional Identification (IRAI) checkbox introduces an added level of customization. 
Upon enabling this checkbox, users gain access to two input fields: a dropdown for choosing an identifier qualifier and an alphanumeric field for entering the associated data. The dropdown includes options such as State License Number, Medicare Provider Number, Medicaid Provider number, and more.
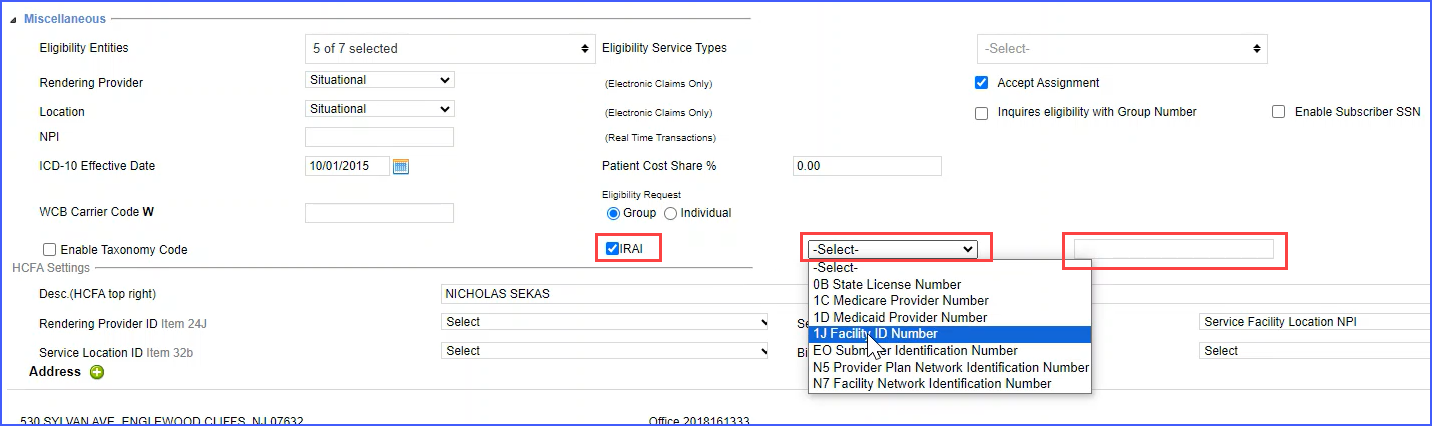
Once relevant data has been entered, it can be stored by clicking the ‘Save’ button.
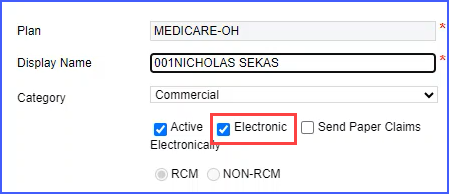
This checkbox is initially unchecked and only appears for plans that are linked to mapped and electronic payers. To enable visibility, the plan must be mapped using the ‘Map’ button at the top, and the ‘Electronic’ checkbox under the ‘Category’ section must also be activated.
The system also maintains logs of any IRAI field changes made.