What is Meant By PAN?
Patients often need to have a ‘Pre-Authorization Number’ (PAN) from their respective plans if there is a procedure that requires clearance. A PAN is sometimes required by the insurance payer/plan.
The following information should be documented in the ‘Authorization’ section of the referrals: ‘Time Limit’, ‘Limit on the number of visits’ or ‘a combination of both options’.
Follow the above mentioned workflow to land on the Referrals tab.
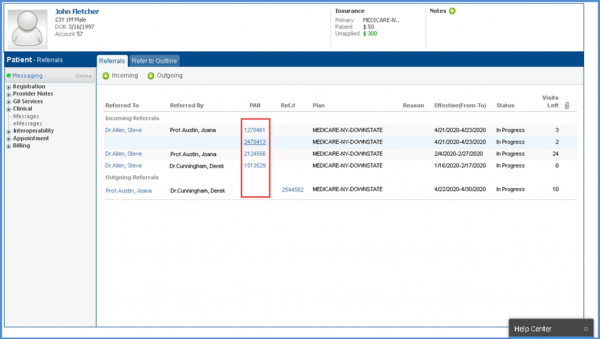
User can view/edit a Referral by clicking the ‘PAN’ hyperlink in the list.![]()
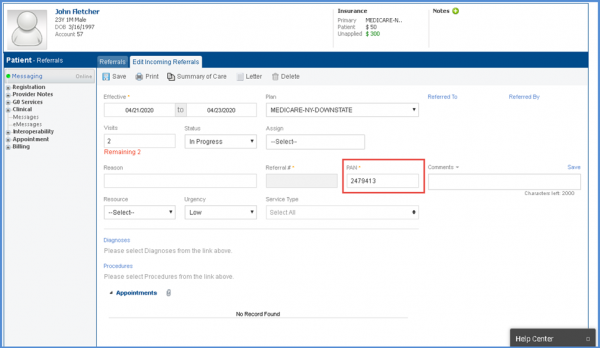
Edit Referral window opens up allowing user to make the required changes.
The ‘Referred to’ and ‘Referred by’ fields are not mandatory and the system lets the user save this information without entering the providers’ names.
Similarly, users can view/edit referrals by clicking the Ref# hyperlink.
Enhancements in ‘Referrals’ and ‘PAN’ have been made in ‘Scheduler’. To view more, click here.
.
