What Information is Displayed on Improvement Activities Dashboard?
Follow the above mentioned workflow to land on the ‘Overview’ tab.
Select the required entity from the ‘Entity’ dropdown
Click ‘Improvement Activities’ tab to display details.
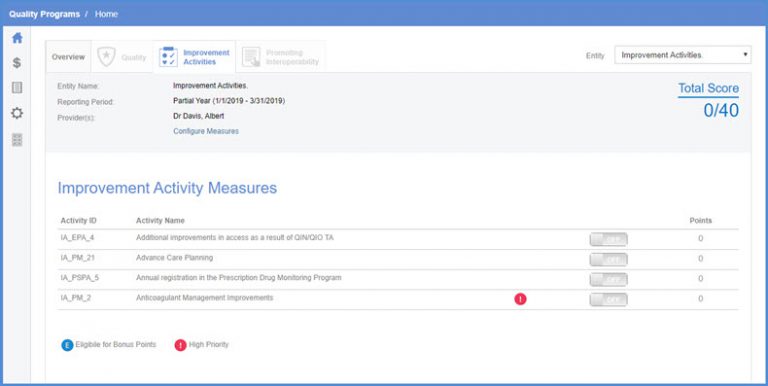
Here, the header displays the following:
- ‘Entity Name’
- ‘Reporting Period’
- ‘Providers’
- Total score of the PI category.
The header remains fixed and can be seen on the ‘Patient List’ screen as well.
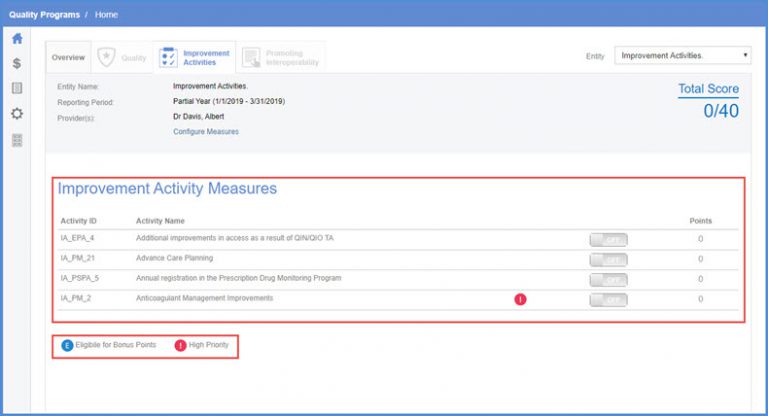
On this tab, users can view the following:
- ‘Activity Id’
- ‘Activity Name’
- Toggle button
- ‘Points’ against each Activity ID.
To add the score, turn on the toggle button.
The icon next to the activity name displays the following:
- If activity is a high priority activity or not
If the activity is eligible for bonus points or not.
Click the ‘Measures’ icon to display a list of measures.
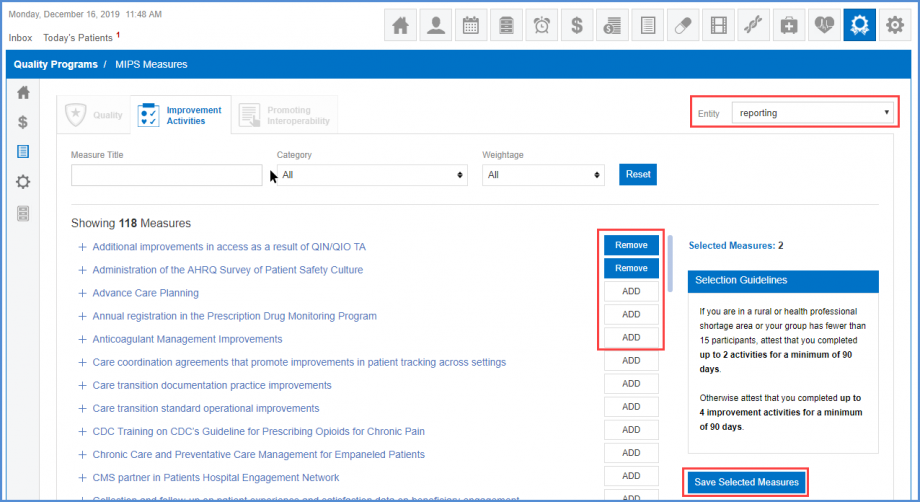
Users can view/select improvement activity measures for MIPS 2020 reporting period. This helps in reporting data on these measures and receive monetary incentives.
The improvement activity measures for MIPS 2020 are enlisted here. When no entity is selected the space in front of the measures remains blank.
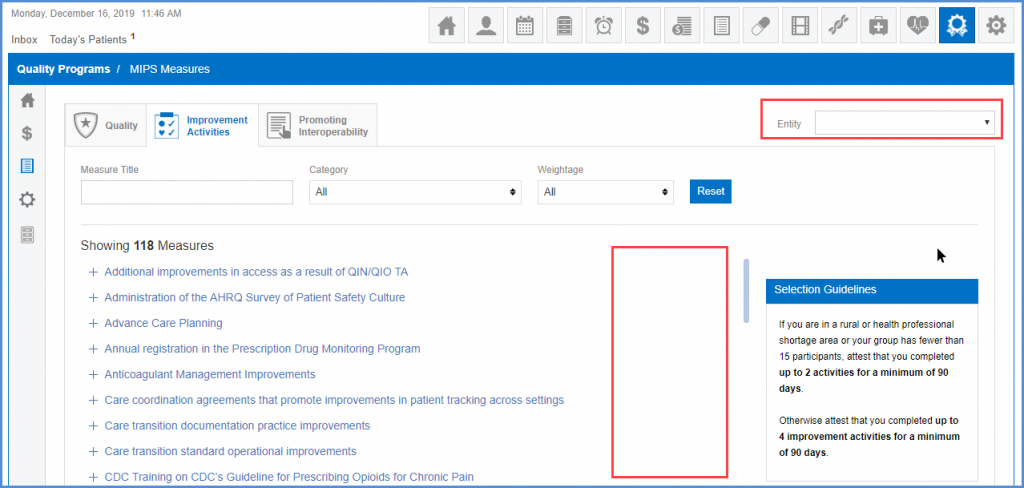
Users can select an entity to view option to add/edit the measure for that entity.
Click here to see how to add measures for Promoting Interoperability.
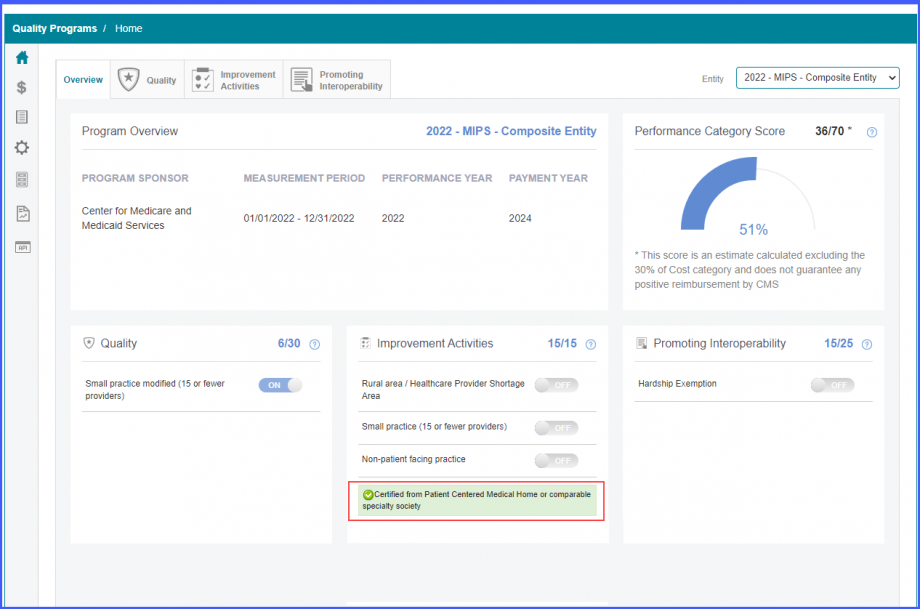
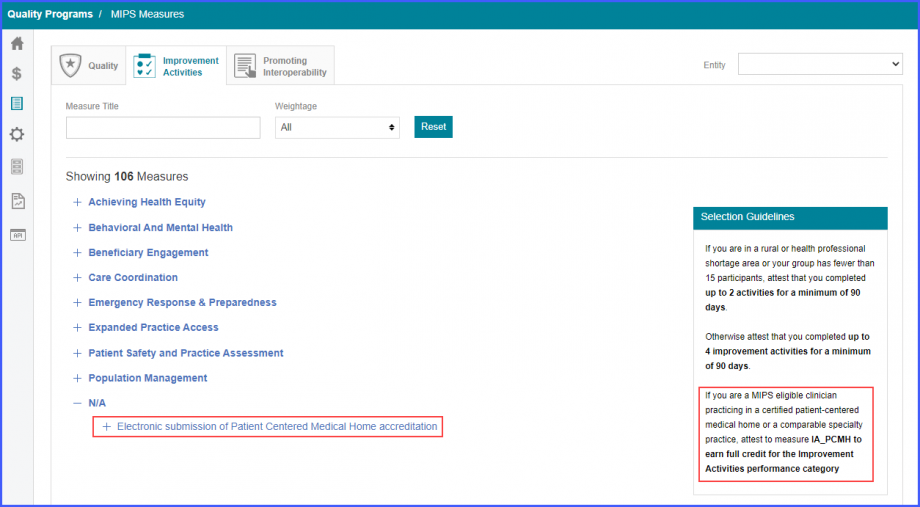
Uses can attest to IA_PCMH measure in the improvement activity category of MIPS Program.![]()
This allows users to earn full credits for improvement activities and receive incentives from CMS.
In the ‘Selection Guidelines’ section, the system displays a text saying:
‘If you are a MIPS eligible clinician practicing in a certified patient-centered medical home or a comparable specialty practice, attest to measure IA_PCMH to earn full credit for the Improvement Activities performance category’
If IA_PCMH measure is selected in an entity for the performance year 2022, then the user receives full 40 pts for the ‘Improvement Activity’ category.
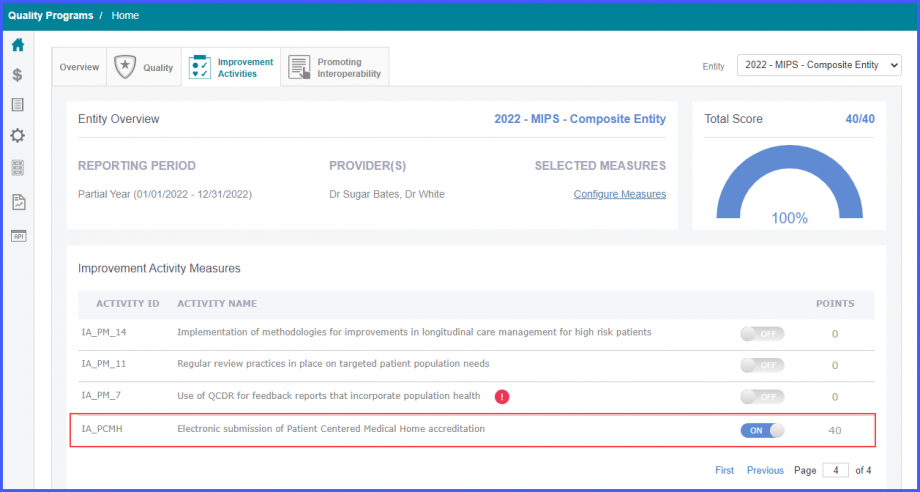
Moreover, the system displays the IA_PCMH attestation on the MIPS Dashboard under the Improvement Activity Section.