What is the Interpretation Feature?
The application has an ‘Interpretation’ feature which is basically a translation table that takes all the Responses from the Electronic Clearinghouse (REC) and from the Insurance Plan (INS).
Furthermore, it helps Interpret their meanings to make them easier to understand for the user, Maps to the location of the exact section and fields that need to be corrected and displays them in the appropriate section (Complete, Incomplete, Processed, Rejected) so that corrections can be made quickly and easily
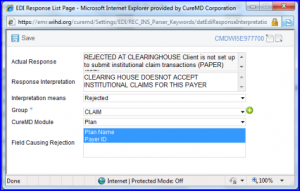
EDI Response Page
Here, Actual response shows exact rejection description from the REC or INS.
Response Interpretation conveys simpler description of the rejection. Interpretation means shows the description which is supposed to be processed or rejected.
Finally, Group, CureMD Module, Field Causing Rejection maps the description to the section, area, and field
Usually, the user does not need to go to this section. However, there may be some cases where the rejection message was so cryptic that it was misunderstood and mapped to the wrong field. In such an instance, if user wants to see the actual response received, user could search for it in either the REC or INS responses. And, as is with the rest of the application, the ‘Advanced Search’ lets user use more than one criteria in the search.
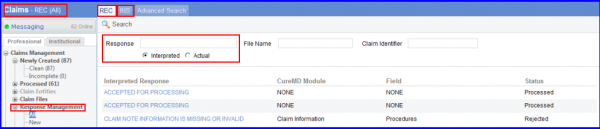
In this section, user can search for All responses (actual or interpreted). Or, specific responses like New responses, Processed (Claims that were processed) and Rejected (Claims that were rejected).
The Rejection Reasons is used by the interpretation team so associated sections are grouped together. An easy way to keep an eye on user’s most frequent rejections (so user knows what areas to review with his team to prevent these errors) user can setup a ‘Rejection Reason KPI’. To setup a ‘Rejection Reason KPI’ click here.
