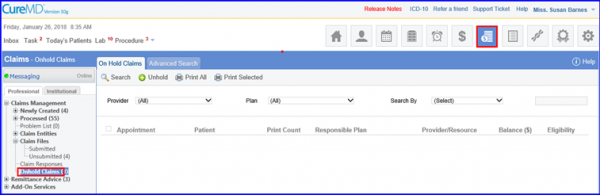
How to Inquire Eligibility for On Hold Claims?
In the CureMD application, users can inquire eligibility for the on-hold claims.
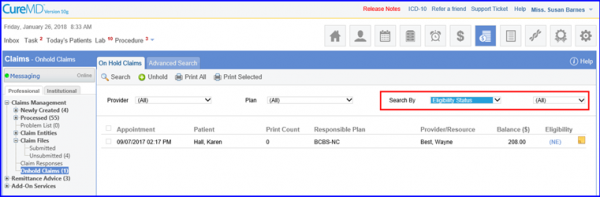
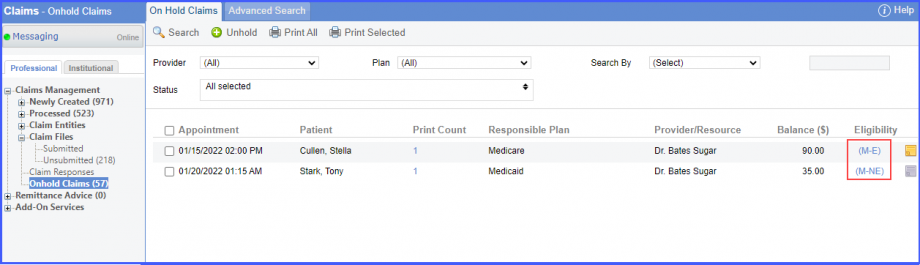
Select ‘Eligibility Status’ from the ‘Search By’ dropdown. This action allows the users to search according to eligibility statuses.
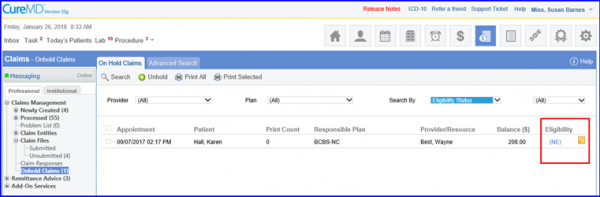
A column named ‘Eligibility’ displays the eligibility status for a patient. Clicking on a status hyperlink opens the ‘Eligibility Inquiry’ tab.
Moreover, user can search for claims using ‘Search By’ dropdown. Claims can be searched by ‘Eligibility Status’ and ‘Program Code’.
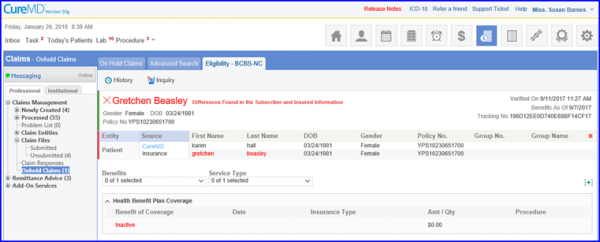
Users can mark a patient eligible or not eligible for insurances that offer real-time benefit check.
This allows billers to perform manual claim validation in case of any issue in the automatic real-time eligibility inquiry.
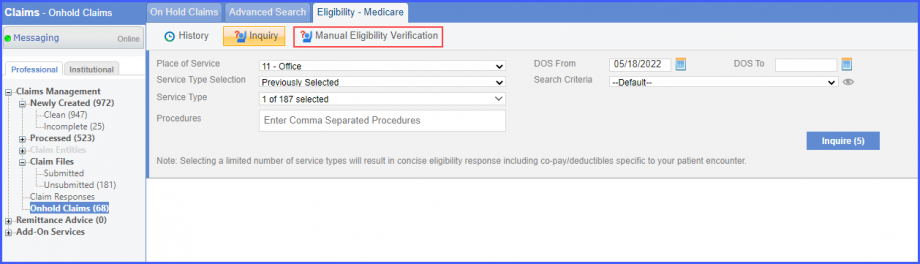
Click on the eligibility status link of an insurance that offers real-time benefit check to open the ‘Eligibility’ tab. Here, the system displays ‘Manual Eligibility Verification’ button next to ‘Inquiry’ button in the top bar.
Clicking ‘Manual Eligibility Verification’ button displays a dropdown screen where a patient can be marked either ‘Eligible’ or ‘Not Eligible’ by selecting the respective radio buttons.
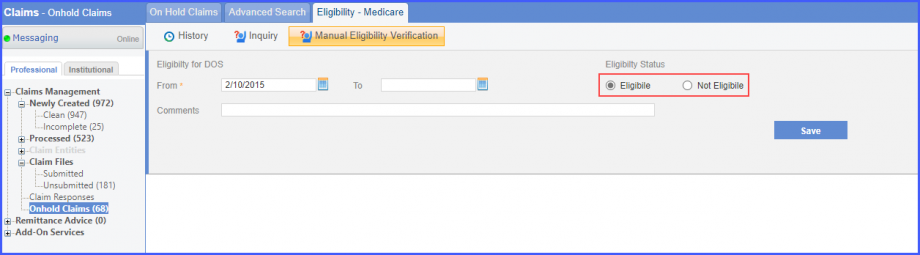
Once done, click ‘Save’ and the system displays a prompt stating:
‘Eligibility status has been set’
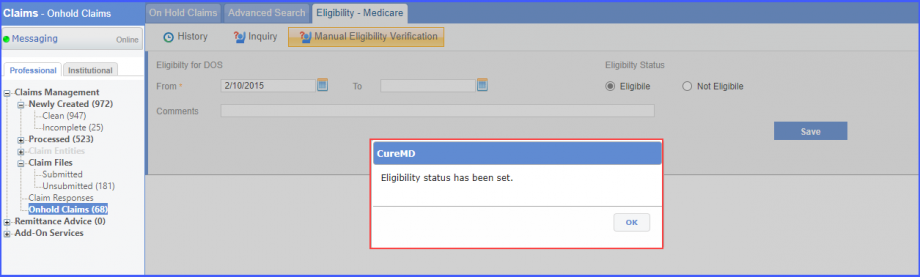
Click ‘OK’ to proceed.
Once the status has been changed, the system displays ‘Manual-E’ eligibility status in the insurance listing if the patient is manually marked as eligible, and ‘Manual-NE’ if marked not-eligible.
The system restricts users from sending requests for eligibility inquiries if the ‘DOS (Date of Service) From’ is older than 364 days.![]()
This ensures eligibility inquiries are requested in a timely manner.
The user has selected a date on the ‘DOS From’ calendar that is older than a year.
A prompt is displayed that states ‘Eligibility can only be inquired for the last 365 days from today’.
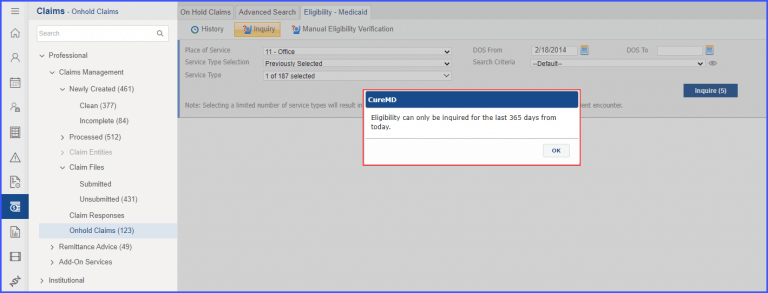
Click the ‘Ok’ button to close the prompt.
If the user selects a date for the ‘DOS From’ field that is within the time period of the past one year, then the eligibility inquiry request is sent successfully.
