Billing FAQs
Telemedicine Services:
Telehealth refers to the delivery of clinical services from a distance. The practice of telehealth largely breaks down into three types of solutions, store-and-forward, remote patient monitoring, and real-time tele encounters.
Interactive – real-time audio/visual (Mostly used)
Store and Forward – asynchronous: Primary Care Providers share patient medical information like lab reports, imaging studies, videos, and other records with another physician, radiologist, or specialist at another location.
Remote Patient Monitoring – (Specialists tracking a patient’s vital signs and activities from at a distance. It is used for high-risk patients, like those with heart conditions and people who have recently been released from the hospital.
- Physicians
- Nurse Practitioners
- Physician Assistants
- Nurse-midwives
- Clinical Nurse Specialists
- Certified Registered Nurse Anaesthetists
- Clinical psychologists and social workers*
- Registered dietitians or nutrition professional
Under the 1135 waiver, effective for services starting March 6, 2020, and for the duration of the COVID-19 Public Health Emergency, Medicare will make payments for Medicare telehealth services rendered to patients in broader circumstances.
Medicare will make payments for professional services rendered to beneficiaries in all areas of the country in all settings. The requirements regarding the ‘originating and distant’ site have been waived during this period.
Under the waiver, eligibility limitations on Medicare patients are to be removed during the emergency. In particular, patients outside of rural areas, and patients in their homes will be eligible for telehealth services, effective March 6, 2020.
The following CMS list highlights all services that may be performed via telemedicine.
https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes.
These services are described by HCPCS codes and paid under the Physician Fee Schedule. Under the emergency declaration and waivers, these services may be provided to patients by professionals regardless of a patient’s location.
- Physician interpretation of diagnostic tests,
- Evisits
- Virtual check-ins
Section 1135(g)(3)) requires that the patient must have a prior established relationship with a practitioner, HHS will NOT conduct audits for prior relationship for claims submitted during this public health emergency.
Currently, CMS allows the use of telecommunications technologies that have audio and video capabilities that are used for two-way, real-time, interactive communication.
Generally, it depends on whether the practice wants to record or not . Reimbursement is always based on documentation for medically necessary services, so accurate documentation is recommended to avoid future issues Recordings are expensive but can help with future audits.
Yes, during COVID-19 emergency providers are allowed to see out-of-state patients.
Yes, verbal consent is required from the patient.
No, CMS has relaxed the HIPAA rules during the emergency.
Yes. The waiver temporarily eliminates the requirement that the originating site must be a physician’s office or other authorized healthcare facility and allows Medicare to pay for telehealth services even when beneficiaries are at their homes or any other care setting .
| G0425-G0427 –Emergency department consultations
G0406-G0408 –Hospital or SNFs consults G0442-G0447 –Alcohol screenings 99406-99407 – smoking cessation 96160-96161 – Health Risk Assessments 97802 -97804 – Medical Nutrition 90832 – 90838 – Psytx pt&/fam 99201-99215 – Office E & M 99231-99233 – Hospital Follow-Ups (1 every 3 days) 99307-99310 – SNF visits (limited to 1 every 30 days) 90791- 90792 -Psych evaluation 90845 – 90846 – Family psytx 90951 – 90970 – Esrd home pt serv |
|
| G0425-G0427 –Emergency department consultations
G0406-G0408 –Hospital or SNFs consults G0442-G0447 –Alcohol screenings 99406-99407 – smoking cessation 96160-96161 – Health Risk Assessments 97802 -97804 – Medical Nutrition 90832 – 90838 – Psytx pt&/fam 99201-99215 – Office E & M 99231-99233 – Hospital Follow-Ups (1 every 3 days) 99307-99310 – SNF visits (limited to 1 every 30 days) 90791- 90792 -Psych evaluation 90845 – 90846 – Family psytx 90951 – 90970 – Esrd home pt serv |
|
No, there are no special requirements. Telehealth services should be documented in the same way as regular services with an indication that the visit was conducted via telehealth.
CMS is not requiring additional or different modifiers associated with telehealth services rendered under these waivers. However, consistent with current rules, there are three scenarios where modifiers are required on Medicare telehealth claims:
First, when a telehealth service is rendered via asynchronous (store and forward) technology as part of a federal telehealth demonstration project in Alaska and Hawaii, the GQ modifier is required;
Second, when a telehealth service is billed under CAH Method II, the GT modifier is required;
Finally, when telehealth service is rendered for purposes of diagnosis and treatment of an acute stroke, the G0 modifier is required.
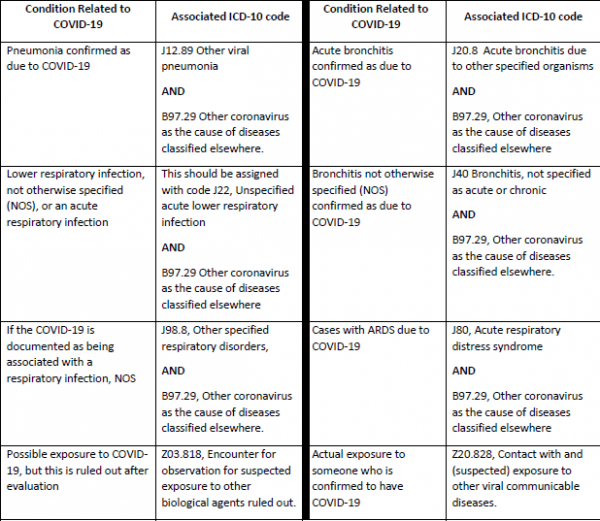
Currently, there are no specific ICD-10 codes to use when billing for services related to COVID-19. The CDC has provided the following coding guidelines for COVID-19.
No, they are not the same.
Telehealth services require both audio and video connection between the provider and the patient.
Telephonic assessment services require only an audio connection between the provider and the patient.
Telephonic codes: 99441 (5 to 10 mins.), 99442(11 to 20 mins.), 99443 (21 to 30 mins.), and for Medicare patients – G2012 (5 to 10 mins.)
The HCFA 1500 should reflect the Place of Service (POS) code 02-Telehealth, to indicate that the billed service was rendered at a professional telehealth service site.
GT: used to indicate a service was rendered via synchronous telecommunication.
GQ: used to indicate a service that was delivered via an asynchronous telecommunications system.
95: Synchronous Telemedicine Service rendered via real-time interactive audio and video telecommunications system.
Medicare pays the same amount for telehealth services as it would if the services were rendered in person.
Medicare uses the facility payment rate when services are rendered via telehealth.
Yes, Medicare advantage plans are required to cover all services which are covered by Medicare.
However, telemedicine services eligibility vary for commercial payers .
Yes, the use of telehealth does not change the out of pocket costs for beneficiaries of Medicare. Beneficiaries are generally liable for their deductible and coinsurance; however, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
Copays and deductibles for telemedicine vary for commercial payers
The telehealth waiver will be effective until the Public Health Emergency declared by the Secretary of Health & Human Services ends.
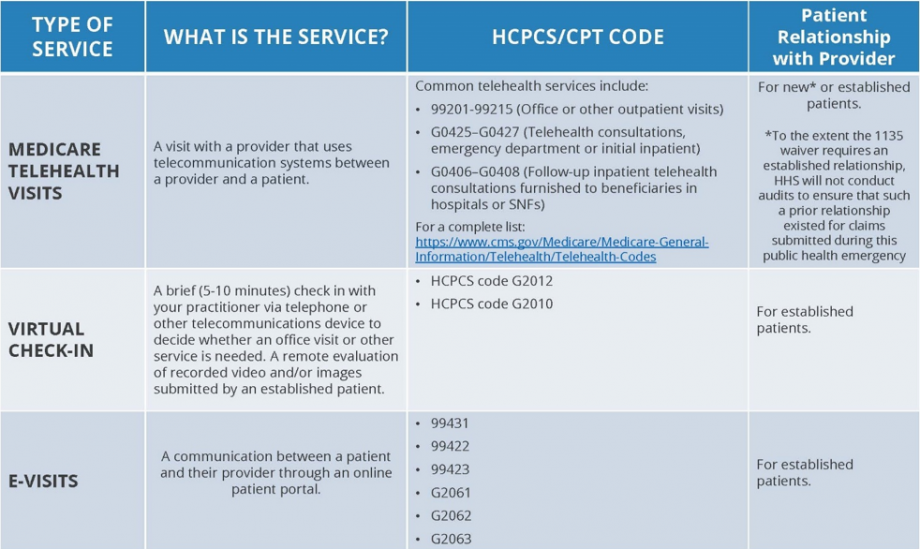
A virtual check-in pays professionals for brief (5 to 10 min) communication that mitigates the need for an in-person visit, whereas a visit rendered via telehealth is treated the same as an in-person visit, and can be billed using the code for that service, using the place of service 02 code to indicate that the service was performed via telehealth.
An e-visit is when a beneficiary communicates with their doctors through online patient portals. But many people are using this word for telemedicine visits as well.
No. The statutory provision broadens telehealth flexibility without regard to the diagnosis of the patient.
Virtual Check-Ins:
In all areas (not just rural), established Medicare patients in their home may have brief communications with practitioners via different technology methods, including synchronous discussion over a telephone or exchange of information through video or image.
These virtual check-ins are for patients with an established (or existing) relationship with a physician or certain practitioners where the communication is not related to a medical visit within the previous 7 days and does not lead to a medical visit within the next 24 hours (or soonest appointment available). The patient must verbally consent to receive virtual check-in services.
Yes, Medicare coinsurance and deductibles would generally apply to these services.
HCPCS code G2012: Brief communication technology-based service, e.g. virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related e/m service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion.
HCPCS code G2010: Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related e/m service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment.
E-Visits:
Patients communicate with their doctors without going to the doctor’s office by using online patient portals.
These services can only be reported when the billing practice has an established relationship with the patient.
Individual services need to be initiated by the patient; however, practitioners may educate beneficiaries on the availability of the service prior to patient initiation.
This is not limited to only rural settings. There are no geographic or location restrictions for these visits.
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable.
Yes, Medicare coinsurance and deductibles would generally apply to these services.
Summary of Medicare Telemedicine Services
Medicare fee schedule for covered Telemedicine services
| Code | Short Descriptor | National Fee | Code | Short Descriptor | National Fee |
| 90785 | Psytx complex interactive | $14.07 | 99214 | Office/outpatient visit est | $80.48 |
| 90791 | Psych diagnostic evaluation | $127.76 | 99215 | Office/outpatient visit est | $113.68 |
| 90792 | Psych diag eval w/med srvcs | $142.91 | 99231 | Subsequent hospital care | $40.06 |
| 90832 | Psytx pt&/family 30 minutes | $63.88 | 99232 | Subsequent hospital care | $73.62 |
| 90833 | Psytx pt&/fam w/e&m 30 min | $66.40 | 99233 | Subsequent hospital care | $106.10 |
| 90834 | Psytx pt&/family 45 minutes | $85.17 | 99307 | Nursing fac care subseq | $44.75 |
| 90836 | Psytx pt&/fam w/e&m 45 min | $84.09 | 99308 | Nursing fac care subseq | $70.37 |
| 90837 | Psytx pt&/family 60 minutes | $127.40 | 99309 | Nursing fac care subseq | $92.75 |
| 90838 | Psytx pt&/fam w/e&m 60 min | $110.43 | 99310 | Nursing fac care subseq | $136.78 |
| 90839 | Psytx crisis initial 60 min | $133.17 | 99354 | Prolonged service office | $124.15 |
| 90840 | Psytx crisis ea addl 30 min | $63.88 | 99355 | Prolonged service office | $93.47 |
| 90845 | Psychoanalysis | $91.31 | 99356 | Prolonged service inpatient | $94.19 |
| 90846 | Family psytx w/o patient | $102.86 | 99357 | Prolonged service inpatient | $94.92 |
| 90847 | Family psytx w/patient | $106.83 | 99406 | Behav chng smoking 3-10 min | $12.63 |
| 90951 | Esrd serv 4 visits p mo <2yr | $959.98 | 99406 | Smoking cessation 3-10 min | $12.63 |
| 90952 | Esrd serv 2-3 vsts p mo <2yr | $0.00 | 99407 | Behav chng smoking > 10 min | $26.71 |
| 90954 | Esrd serv 4 vsts p mo 2-11 | $832.59 | 99407 | Smoking cessation >10 min | $26.71 |
| 90955 | Esrd srv 2-3 vsts p mo 2-11 | $469.16 | 99495 | Trans care mgmt 14 day disch | $125.59 |
| 90957 | Esrd srv 4 vsts p mo 12-19 | $660.44 | 99496 | Trans care mgmt 7 day disch | $165.65 |
| 90958 | Esrd srv 2-3 vsts p mo 12-19 | $448.59 | 99497 | Advncd care plan 30 min | $80.48 |
| 90960 | Esrd srv 4 visits p mo 20+ | $291.24 | 99498 | Advncd are plan addl 30 min | $75.79 |
| 90961 | Esrd srv 2-3 vsts p mo 20+ | $244.69 | G0108 | Diab manage trn per indiv | $57.02 |
| 90963 | Esrd home pt serv p mo <2yrs | $557.95 | G0109 | Diab manage trn ind/group | $15.88 |
| 90964 | Esrd home pt serv p mo 2-11 | $487.93 | G0270 | Mnt subs tx for change dx | $29.23 |
| 90965 | Esrd home pt serv p mo 12-19 | $466.28 | G0296 | Visit to determ ldct elig | $27.79 |
| 90966 | Esrd home pt serv p mo 20+ | $244.33 | G0396 | Alcohol/subs interv 15-30mn | $33.92 |
| 90967 | Esrd home pt serv p day <2 | $18.41 | G0397 | Alcohol/subs interv >30 min | $66.04 |
| 90968 | Esrd home pt serv p day 2-11 | $16.24 | G0406 | Inpt/tele follow up 15 | $39.70 |
| 90969 | Esrd home pt serv p day 12-19 | $15.52 | G0407 | Inpt/tele follow up 25 | $73.26 |
| 90970 | Esrd home pt serv p day 20+ | $8.30 | G0408 | Inpt/tele follow up 35 | $105.38 |
| 96116 | Neurobehavioral status exam | $86.62 | G0420 | Ed svc ckd ind per session | $114.40 |
Medicare fee schedule for covered Telemedicine services
| Code | Short Descriptor | National Fee | Code | Short Descriptor | National Fee |
| 96156 | Health behavior assessment | $90.58 | G0421 | Ed svc ckd grp per session | $26.71 |
| 96158 | Health behavior intervention | $61.71 | G0425 | Inpt/ed teleconsult30 | $101.77 |
| 96159 | Health behavior intervention, additional 15 | $21.29 | G0426 | Inpt/ed teleconsult50 | $138.22 |
| 96160 | Pt-focused hlth risk assmt | $2.53 | G0427 | Inpt/ed teleconsult70 | $204.99 |
| 96161 | Caregiver health risk assmt | $2.53 | G0438 | Ppps, initial visit | $172.87 |
| 96164 | Health behavior intervention, group | $9.02 | G0439 | Ppps, subseq visit | $117.29 |
| 96165 | Health behavior intervention, group | $3.97 | G0442 | Annual alcohol screen 15 min | $9.74 |
| 96167 | Health behavior intervention, family | $66.04 | G0443 | Brief alcohol misuse counsel | $24.18 |
| 96168 | Health behavior intervention, family | $23.46 | G0444 | Depression screen annual | $9.74 |
| 97802 | Medical nutrition indiv in | $34.65 | G0445 | High inten beh couns std 30m | $24.18 |
| 97803 | Med nutrition indiv subseq | $29.23 | G0446 | Intens behave ther cardio dx | $24.18 |
| 97804 | Medical nutrition group | $16.24 | G0447 | Behavior counsel obesity 15m | $24.18 |
| 99201 | Office/outpatient visit new | $27.07 | G0459 | Telehealth inpt pharm mgmt | $42.59 |
| 99202 | Office/outpatient visit new | $51.61 | G0506 | Comp asses care plan ccm svc | $46.56 |
| 99203 | Office/outpatient visit new | $77.23 | G0508 | Crit care telehea consult 60 | $214.37 |
| 99204 | Office/outpatient visit new | $132.09 | G0509 | Crit care telehea consult 50 | $197.77 |
| 99205 | Office/outpatient visit new | $172.51 | G0513 | Prolong prev svcs, first 30m | $62.80 |
| 99211 | Office/outpatient visit est | $9.38 | G0514 | Prolong prev svcs, addl 30m | $62.80 |
| 99212 | Office/outpatient visit est | $26.35 | G2086 | Off base opioid tx first m | $301.35 |
| 99213 | Office/outpatient visit est | $52.33 | G2087 | Off base opioid tx, sub m | $293.77 |
| G2088 | Off opioid tx month add 30 | $35.01 |
Medicare fee schedule for covered Telemedicine services
| Code | Short Descriptor | National Fee | Code | Short Descriptor | National Fee |
| 99421 | Online E &M service, 5-10 mint | $13.35 | G2061 | Nonphysician online assessment 5-10 mint | $12.27 |
| 99422 | Online E &M service, 11-20 mint | $27.43 | G2062 | Nonphysician online assessment 11-20 mint | $21.65 |
| 99423 | Online E &M service, >21 mint | $43.67 | G2063 | Nonphysician online assessment > 20 mint | $33.56 |
Medicare fee schedule for covered Virtual Check-ins
| Code | Short Descriptor | National Fee | Code | Short Descriptor | National Fee |
| G2012 | Virtual check-in 5-10 minutes | $13.35 | G2013 | Remote evaluation of recorded video/image | $9.38 |
Note: As part of the current waiver, payers can cover even more codes that are not listed here. If the service you are opting to deliver by telehealth are not listed above, please contact the respective insurance for verification.
Commercial Insruance and Telemedicine:
Yes, almost all insurances cover telemedicine services. However, coverage can vary depending on the patient’s plan.
No, following the HHS 1135 waiver, commercial insurances have also removed the restriction of originating and distant sites.
|
99201-99215 – Office E & M 99231-99233 – Hospital Follow-Ups (1 every 3 days) 99307-99310 – SNF visits (limited to 1 every 30 days) 99495-99498 – Transitional care management 99354-99357 – Prolonged care
|
99406-99407 – smoking cessation 96156-96168 – Health Risk Assessments 97802 -97804 – Medical Nutrition 90832 – 90838 – Psytx pt&/fam 90791- 90792 -Psych evaluation 90845 – 90846 – Family psytx 90951 – 90970 – Esrd home pt serv |
Note: As part of the current waiver, payers can cover even more codes that are not listed here. If the services you are opting to deliver by telehealth are not listed above, please contact the respective insurance for verification.
The payment would vary from insurance to insurance and from patient to patient. Providers can contact individual commercial insurances to find out the contracted amount.
Yes, referral or authorization is required just like face-to-face services. However, after the national emergency declared by the US gov’t., many insurances have relaxed their requirements for referrals or authorization requirements.
Yes, the use of telehealth does not change the out of pocket costs for beneficiaries. Beneficiaries are generally liable for copay, deductible and coinsurance; however, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by insurances.
Commercial insurances that cover telemedicine
| Insurance | Cover Telemedicine? | Billable Codes | Modifier(s) | POS |
| Aetna | Yes | Medicare Approved | — | 2 |
| Anthem | Yes | Medicare Approved | GT / 95 | 2 |
| BCBS FL | Yes | Medicare Approved | GT / 95 | 2 |
| BCBS ID | Yes | Medicare Approved | GT / 95 | 2 |
| BCBS NC | Yes | Medicare Approved | GT / 95 | 2 |
| BCBS NV | Yes | Medicare Approved | GT / 95 | 2 |
| BCBS NY | Yes | Medicare Approved | GT / 95 | 2 |
| Carefirst BCBS | Yes | Medicare Approved | GT / 95 | 2 |
| Cigna | Yes | Medicare Approved | — | 2 |
| Emblem Health | Yes | Medicare Approved | GT / 95 | 2 |
| Fidelis | Yes | Medicare Approved | GT / 95 | 2 |
| GHI | Yes | Medicare Approved | GT / 95 | 2 |
| Health Care Partners | Yes | Medicare Approved | GT / 95 | 2 |
| Health First | Yes | Medicare Approved | GT / 95 | 2 |
| HEALTH PLAN OF NV | Yes | Medicare Approved | — | 2 |
| HEALTHSCOPE | Yes | Medicare Approved | — | 2 |
| HIP | Yes | Medicare Approved | GT / 95 | 2 |
| MERITAIN HEALTH | Yes | Medicare Approved | — | 2 |
| Oxford Health Plan | Yes | Medicare Approved | GT / 95 | 2 |
| Regence | Yes | Medicare Approved | — | 2 |
| Select Health | Yes | Medicare Approved | GT / 95 | 2 |
| Senior Care Plus | Yes | Medicare Approved | — | 2 |
| SIERRA HEALTH AND LIFE | Yes | Medicare Approved | — | 2 |
| STARMARK | Yes | Medicare Approved | — | 2 |
| TRICARE | Yes | Medicare Approved | GT / 95 | 2 |
| TRICARE WEST | Yes | Medicare Approved | GT / 95 | 2 |
| TRIWEST-VAPC3 | Yes | Medicare Approved | GT / 95 | 2 |
| UMR | Yes | Medicare Approved | GT / 95 | 2 |
| UNITED HEALTH CARE | Yes | Medicare Approved | GT / 95 | 2 |
| Value Options | Yes | Medicare Approved | GT / 95 | 2 |
| Wellcare | Yes | Medicare Approved | GT / 95 | 2 |
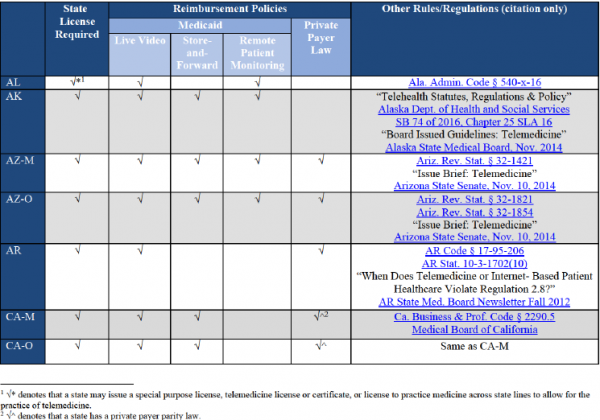
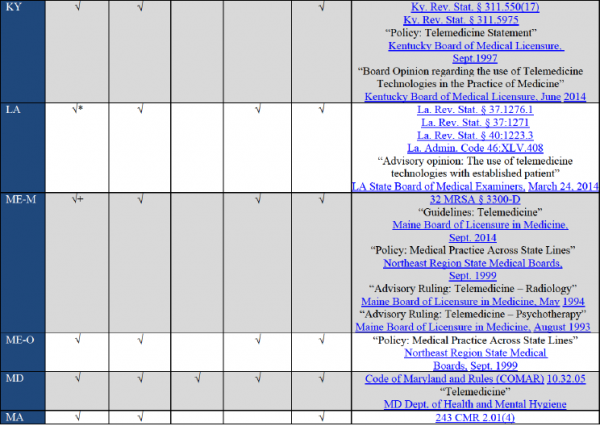
Note: Forty (40) states and the District of Columbia govern private payer telehealth reimbursement policies. This is not a complete list of insurances, but major insurances are included. Practices should call individual insurance payers before delivering services to make sure that their telemedicine services are covered under patient benefits.
The originating site is the location of the patient at the time the service is being furnished. The distant site is the site where the physician or other licensed practitioner delivering the service is located.
Medicaid and Telemedicine Services:
- Forty-nine (49) state boards, plus the medical boards of District of Columbia, Puerto Rico, and the Virgin Islands, require that physicians engaging in telemedicine are licensed in the state in which the patient is located.
- Twelve (12) state boards issue a special purpose license, telemedicine license or certificate, or license to practice medicine across state lines to allow for the practice of telemedicine.
- Six (6) state boards require physicians to register if they wish to practice across state lines.
- All states and the District of Columbia provide reimbursement for some form of live video in Medicaid fee-for-service at the same rate they pay face to face visits.
- Fourteen (14) states reimburse for store-and-forward.
- Twenty-two (22) states reimburse for remote patient monitoring.
- Eight (8) states reimburse for all three, with certain limitations.
|
99201-99215 – Office E & M 99231-99233 – Hospital Follow-Ups (1 every 3 days) 99307-99310 – SNF visits (limited to 1 every 30 days) 99495-99498 – Transitional care management 99354-99357 – Prolonged care
|
99406-99407 – smoking cessation 96156-96168 – Health Risk Assessments 97802 -97804 – Medical Nutrition 90832 – 90838 – Psytx pt&/fam 90791- 90792 -Psych evaluation 90845 – 90846 – Family psytx 90951 – 90970 – Esrd home pt serv |
Note: As part of the current waiver, payers can cover even more codes that are not listed here. If the services that you intend to deliver via telehealth are not listed above, please contact the respective insurance for verification.
Almost all states require the Place of Service code 02- telemedicine along with the GT modifier on the HCFA 1500 claim form.
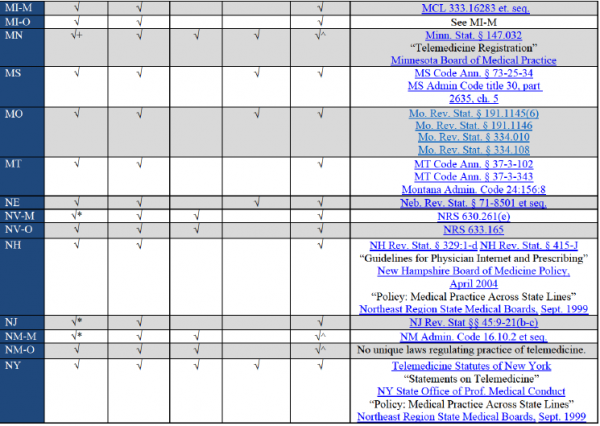
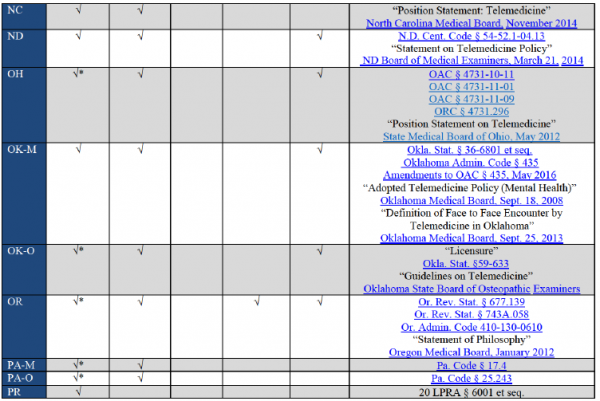
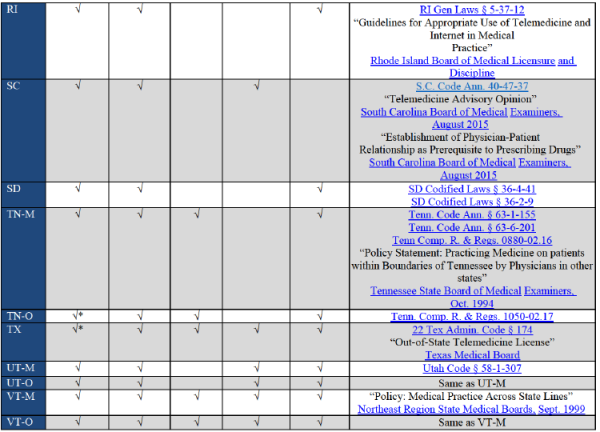
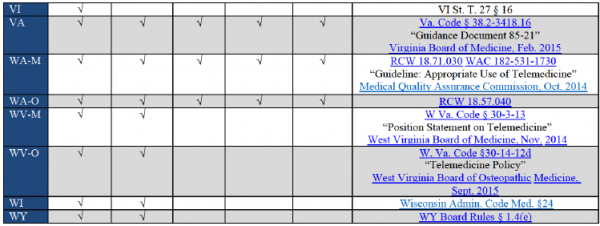
The covered services vary from state to state. Please review the charts given below to find out which state Medicaid covers what services.
For Medicare claims, you can bill claims with just POS 02. But for commercial insurances, you have to check with insurance what are their guidelines on billing telemedicine claims. Do they need GT/95 modifier or submitting claim under POS 02 would be enough.
Please go through below link to check your state guidelines:
https://www.cchpca.org/telehealth-policy/current-state-laws-and-reimbursement-policies#
