How to e-bill Secondary Plans?
On the Payer List, those listed as ‘Payer Accepts COB (electronic Co-ordination Of Benefits)’ or ‘Electronic COB’ can be billed electronically.
1. If not already done, set the plan in CureMD to bill electronically. Configure the desired plan. For example, let’s setup CIGNA PPO.
Firstly, from the payer list look for the Cigna PPO and ID for Professional claims.
The Payer ID is 62308, the EDI version is 5010, and the Payer accepts COB.
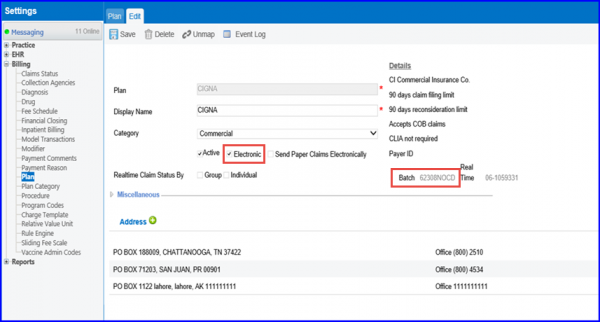
Set the following fields:
- Claim Gateway
- Electronic
- Accept COB Claims
Now check if the Payer provides eligibility:
The payer ID is same, so fill in the Eligibility Gateway with the same Payer Number and click on the ‘Save’ button.
For example, if ABC Insurance can receive electronic claims, but can’t handle COBs, and one of user’s patients has ABC Insurance as their secondary, add plans:
- ABC Insurance (set to bill electronically)
- ABC Insurance Supplemental (to bill on paper)
2. When the primary insurance payment is posted, and the secondary can be billed electronically, the secondary claim will automatically show under:
and can be billed from there. For step by step instructions, please click here.
