How to Address Unbalanced Co-ordination of Benefits?
‘COB’ stands for ‘Co-ordination of Benefits’. This occurs when the patient has more than one insurance and the plans “coordinate” how the claim is to be paid. The two most common reasons for this error are primary payment manually entered with ‘unbalanced payments’ and primary denies the claim but the payment is marked as a denial.
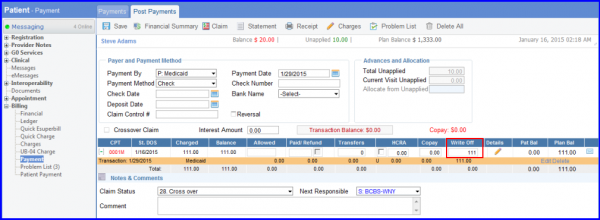
A primary payment is manually entered with ‘unbalanced payments’. ‘Unbalanced payments’ occur when the transaction is mathematically incorrect or has not accounted for all of the money or write-offs in the transaction. For example:
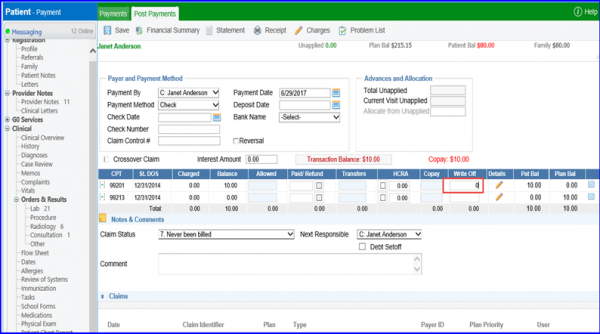
When this payment is entered, the user erased the write-off of $111 that filled in automatically, and changed it to $0. The red Transaction Balance warning tells that $111 has not been applied. If done correctly, the Transaction Balance would be $0.
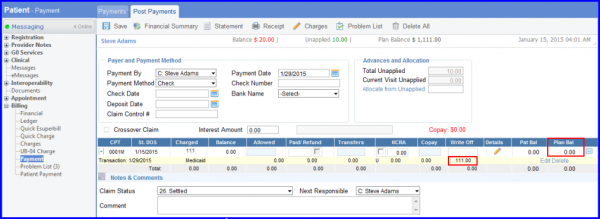
It does not mean that user has to enter the write-off. Usually, the difference between the charge and allowed amounts should be written off. But, sometimes a secondary plan covers it. Transaction can be done like this:
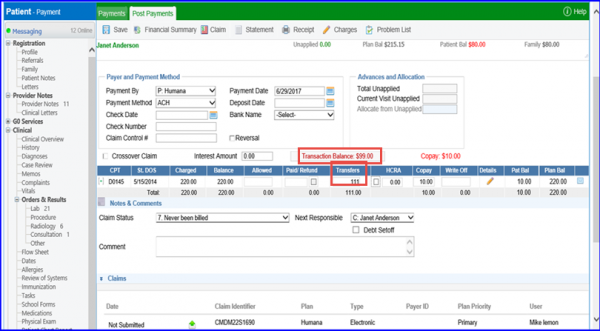
Instead of writing it off, put the $111 in ‘Transfers’ to see if the secondary pays it.
Another way this error is created is when the primary denies the claim but the payment is marked as a denial. When user enters a zero payment and then enters the full amount as a write-off, the application highlights the ‘CPT’ code.
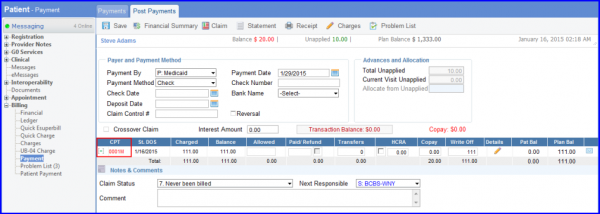
Click on it to see these options:
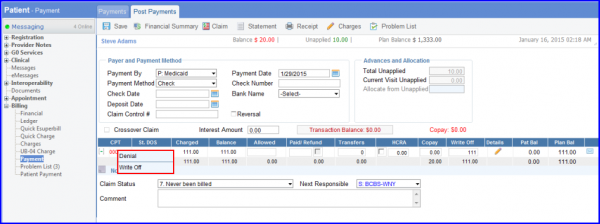
Denial – When user clicks on ‘denial’, the claim is saved as a temporary transaction. This is helpful if user is not sure whether the write-off is appropriate or not and wants to revisit this later.
When user saves it, it will either show in the Denial Management section, be highlighted in orange to show it is a temporary transaction or not affect the claim balance.
To know more about Denial Management click here.
Clicking on ‘Write Off’ confirms it as a normal transaction and the balance is affected.
So, in either of these cases, the payment needs to be corrected and saved before it is billed.
