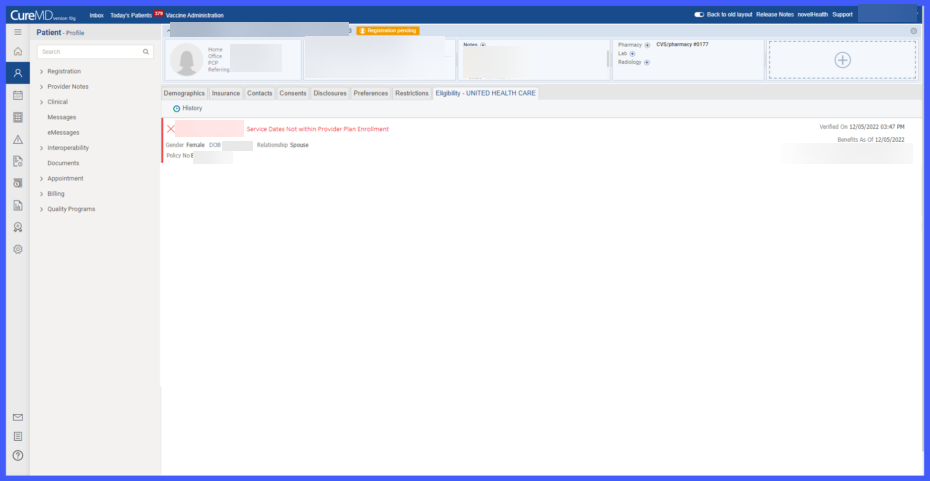
Eligibility Status Update for Non-Provider Plan Dates
With this enhancement in the CureMD application, the system updates the eligibility status to “Not Eligible” when an eligibility response is received as:
- “78 – Subscriber/Insured Not in Group/Plan Identified, Please Correct and Resubmit”
- “52 – Service Dates Not Within Provider Enrollment”
This change enables the user to view accurate eligibility status details and understand the reason for ineligibility.
Eligibility Response: Eligibility Status
When the system receives this eligibility response, it processes this information and updates the status to “Not Eligible.” In this instance, the system displays the message ” Service Dates Not within Provider Plan Enrollment” ensuring users are notified of the specific reason for ineligibility. The response screen remains consistent with existing functionality, displaying relevant details from the request, patient profile, and rejection reason from the response.