CMS2v9 – Preventive Care and Screening: Screening for Depression and Follow-Up Plan
| Preventive Care and Screening: Screening for Depression and Follow-Up Plan | CMS2v9 | Percentage of patients aged 12 years and older screened for depression on the date of the encounter using an age appropriate standardized depression screening tool AND if positive, a follow-up plan is documented on the date of the positive screen. |
|---|---|---|
| DENOMINATOR
All patients aged 12 years or older at the start of the measurement period. And also if a qualifying encounter for depression screening exists for the patient. – DENOMINATOR EXCLUSION Patients with an active diagnosis for Depression or a diagnosis of Bipolar Disorder before the encounter. – NUMERATOR Patients screened for depression on the date of the encounter or up to 14 days prior to the date of the encounter using an age appropriate standardized tool AND if positive, a follow-up plan is documented on the date of the eligible encounter. – DENOMINATOR EXCEPTIONS Patient Reason(s) Patient refuses to participate OR Medical Reason(s) Patient is in an urgent or emergent situation where time is of the essence and to delay treatment would jeopardize the patient’s health status OR Situations where the patient’s cognitive capacity, functional capacity or motivation to improve may impact the accuracy of results of standardized depression assessment tools. For example: certain court appointed cases or cases of delirium. |
||
| – APPLICATION WORKFLOW
For Denominator: All patients aged 12 years and older with at least one eligible encounter during the measurement period are included in denominator.
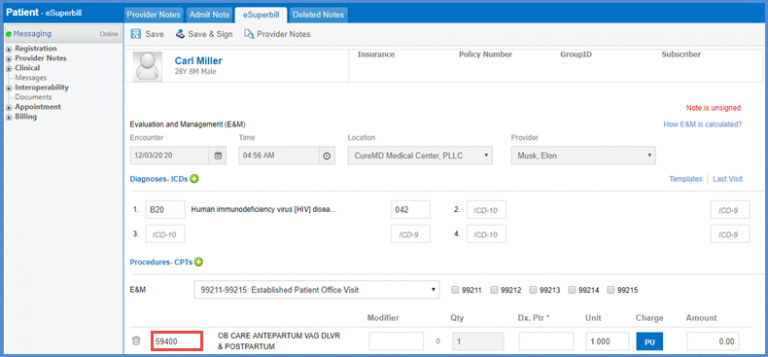
For Numerator: Patients screened for depression on the date of the encounter using an age appropriate standardized tool. Use following workflow to document depression screening: Patient > Clinical > Evaluations Select Adolescent depression screening for patients between the age range of 12 to 17 or Adult depression screening for patients aged over 17. 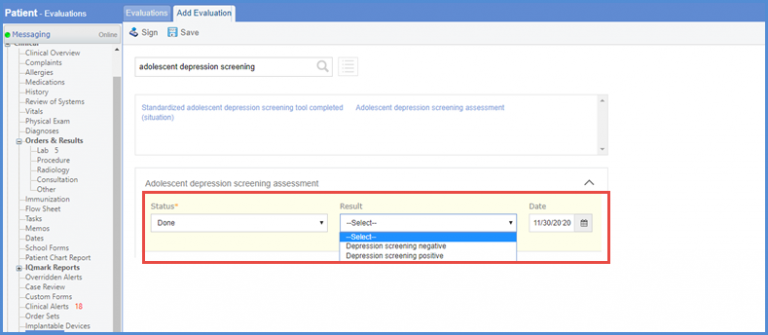
If the result of depression screening is negative then the patient will be included in the numerator without any further action. If the result of depression screening is Positive, then any one of the following must be documented on the date of positive screening.
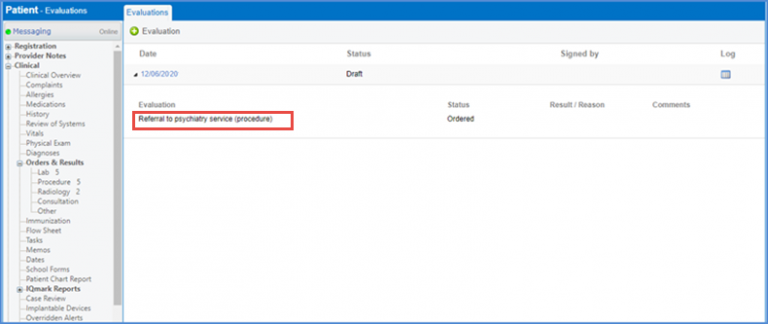
1. Additional evaluation for depression – adolescent/adult: To document depression screening, navigate to Patient > Clinical > Evaluations. Evaluation can be added using relevant evaluation codes. In this case, the evaluation i.e. Assessment for Bipolar Disorder is added using the code 429441000124107. 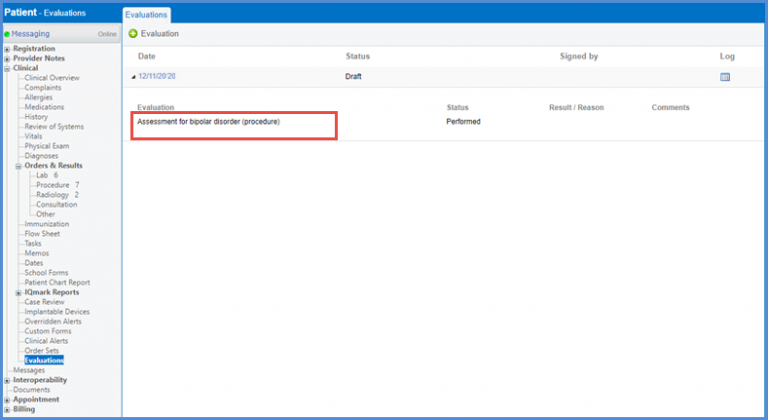 2. Referral for Depression Adolescent/adult: In order to document an outgoing referral, user can navigate to Patient > Clinical > Evaluations.
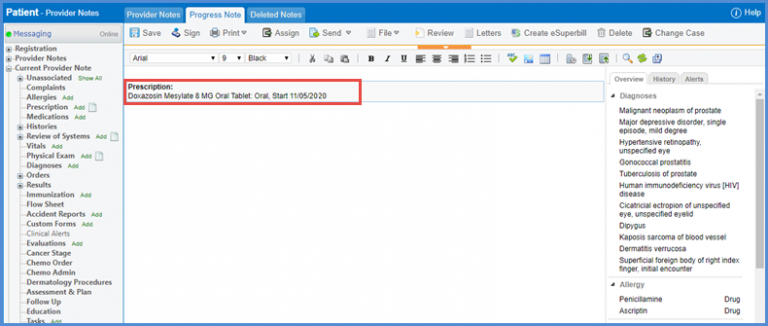
3. Pharmacologic Depression Treatment – adolescent/adult (Prescribed Medications) For documenting medications for depression, navigate to Patient > Provider Notes > Prescriptions. Medication list includes:
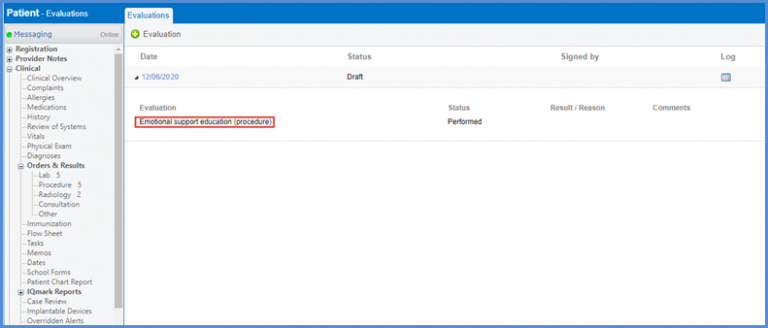
 4. Follow-up for depression – adolescent/adult: To document a follow-up encounter, navigate to Patient > Clinical > Evaluations. To add ‘Emotional Support Education’, the code 385725001 is used.
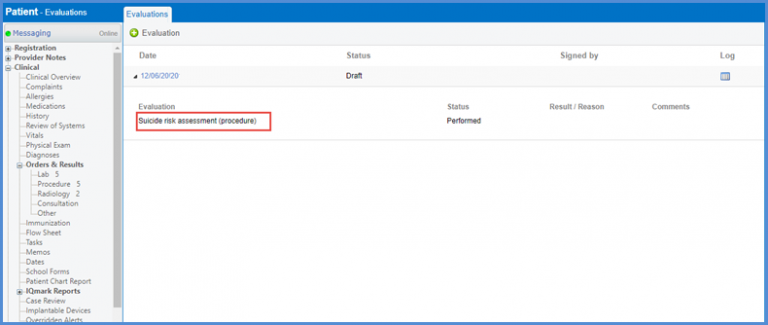
5. Suicide Risk Assessment: To document Suicide Risk Assessment, navigate to Patient > Clinical > Evaluations. In this case, the code ‘225337009’ has been used to add ‘Suicide Risk Assessment’ evaluation.
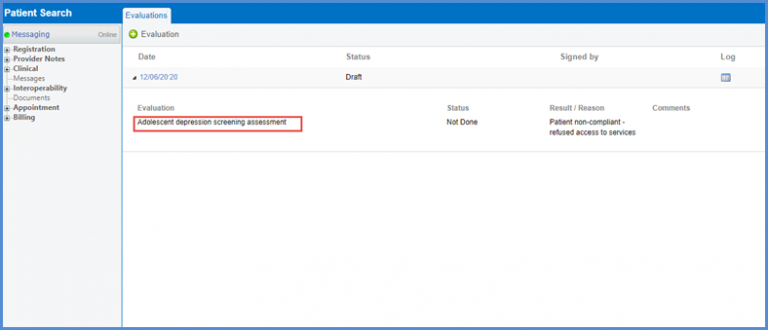
– DENOMINATOR EXCEPTION Patient Reason(s) OR Medical Reason(s) OR Situations where the patient’s cognitive capacity, functional capacity or motivation to improve may impact the accuracy of results of standardized depression assessment tools. For example: certain court appointed cases or cases of delirium. To learn more about How to Document Denials and Refusals, click here.
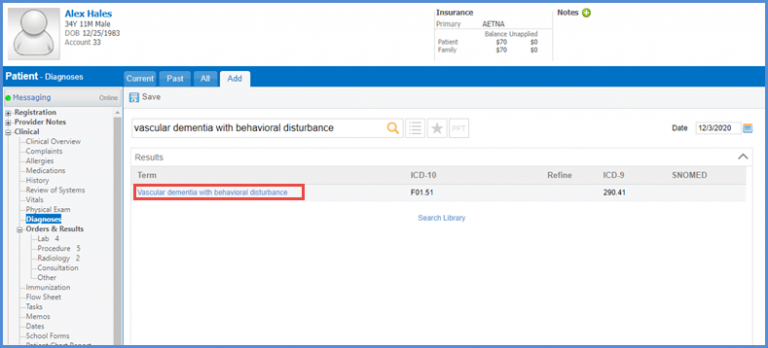
– DENOMINATOR EXCLUSION Patients with an active diagnosis for Depression or a diagnosis of Bipolar Disorder during measurement period.
|
||